High Risk Squamous Cell Carcinoma
High Risk Squamous Cell Carcinoma
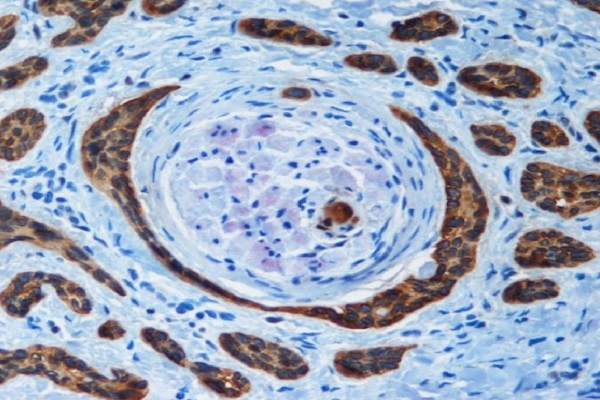
Important high-risk features in cutaneous squamous cell carcinoma (cSCC) include poor differentiation, perineural invasion, tumour size ≥20 mm, location on high-risk areas (e.g., ears, lips), and rapid growth. These features with poor prognostic indicators necessitate more aggressive management strategies to optimise patient outcomes.
Diagnostic techniques like biopsy, histopathology, and imaging modalities (e.g., MRI, CT) to accurately stage the disease, is critical for deciding the extent of treatment. Even sentinel lymph node biopsy is indicated for staging in certain cases.
Based on risk assessment, treatment recommendations include: surgical excision with adequate margins, Mohs micrographic surgery for high-risk locations or recurrent tumours, adjuvant radiotherapy for high-risk features or incomplete excision, and systemic therapies (immunotherapy and targeted therapies) for advanced, metastatic, or inoperable cases.
Regular follow-ups to monitor for recurrence or new primary tumours are important in patients with high-risk cSCC.
Stanganelli, I., Spagnolo, F., Argenziano, G., et al. (2022). "The Multidisciplinary Management of Cutaneous Squamous Cell Carcinoma: A Comprehensive Review and Clinical Recommendations by a Panel of Experts." Cancers, 14(2), 377. doi:10.3390/cancers14020377
END FOR WIDE LOCAL EXCISIONS?
End for Wide Local Excision?
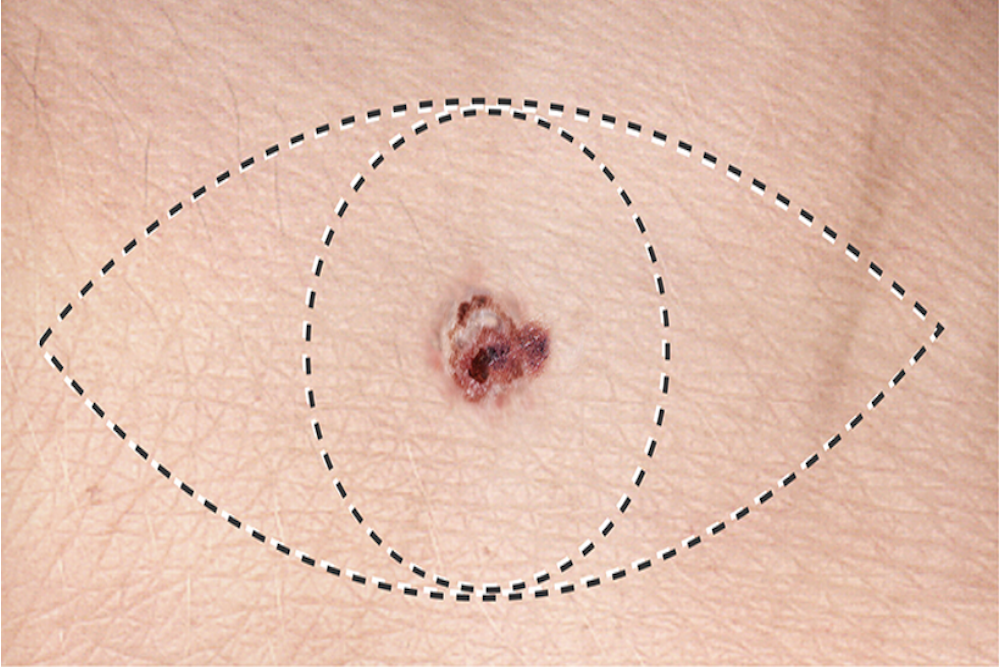
In the journal article referenced below, the authors argue that the current two-step surgical approach for treating cutaneous melanoma, which involves an initial diagnostic excision followed by Wide Local Excision (WLE), may no longer be necessary.
WLE aims to remove potential microscopic melanoma cells around the tumour to prevent recurrence. There is no strong evidence that WLE improves overall survival compared to just a complete diagnostic excision. Studies show a low chance (0-4.2%) of finding melanoma cells in the tissue removed during WLE.
WLE can cause significant scarring and other complications. Advancements in systemic therapy for melanoma may make WLE unnecessary.
Eur J Cancer.2023 Jan:178:82-87.
New Hope for Treatment-Resistant Melanoma
New Hope for Treatment-Resistant Melanoma
Cancer therapy resistance is a major hurdle in medicine, despite advancements in targeted therapies and immunotherapy. Combining different treatments is crucial to overcome this resistance.
Resistance can arise from genetic changes in cancer cells or from them adapting to become "drug-tolerant persisters" (DTPs). These DTPs rely heavily on their mitochondria, the cell's energy centers.
Targeting this mitochondrial function with antibiotics like tetracyclines offers a promising approach to eliminate DTPs and improve treatment outcomes.
Tetracyclines: A Repurposed Weapon Against Melanoma?
Research suggests tetracyclines, a class of older antibiotics, could be repurposed to target therapy-resistant melanoma. These antibiotics may not directly enhance immunotherapy response, but they could be used in combination for melanoma treatment, potentially slowing tumor growth.
J. Exp. Med. 2021 Vol. 218 No. 9
New Vitamin D and Sun Exposure Guidelines

New Vitamin D and Sun Exposure Guidelines
Australian sun exposure recommendations now consider skin type and risk of skin cancer in the Australian and New Zealand Journal of Public Health, February 2024.
People with lighter skin tones (Fitzpatrick I-IV) are at higher risk of skin cancer and should minimise sun exposure during peak UV hours (UV index 3 or higher) and use sun protection. They can still get enough vitamin D with short exposures during non-peak hours.
People with darker skin tones (Fitzpatrick V-VI) have a lower risk of skin cancer and may need more sun exposure to get enough vitamin D. They may not need daily sunscreen but should use it during prolonged sun exposure.
Our doctors can advise on personalised recommendations and vitamin D supplementation if needed. Public health messages will still focus on skin cancer prevention.
Non-Melanoma Skin Cancer killing more people than Melanoma

Non-Melanoma Skin Cancer killing more people than Melanoma
A new study presented at the European Academy of Dermatology and Venerology (EADV) Congress reveals surprising findings about skin cancer. While melanoma is often considered the most dangerous form, non-melanoma skin cancer (NMSC) is now causing more deaths globally.
In 2020, NMSC caused over 63,700 deaths compared to melanoma's estimated 57,000, despite being less likely to spread or be fatal per individual case. This discrepancy is due to the much higher prevalence of NMSC, with nearly 1.2 million reported cases worldwide in 2020 compared to 324,635 melanoma cases.
Fair-skinned, elderly populations in specific countries like the US, Germany, and Australia are most affected, but even darker-skinned populations face significant risk.
To Shave, or not to Shave?

To Shave Or Not to Shave?
Melanoma is the most lethal form of skin cancer. Accurate diagnosis and early treatment are crucial for improving survival. Biopsy is a key step in diagnosis, and while excision biopsy is recommended, some melanomas are diagnosed using shave biopsy (which has a high rate of deep margin positivity, 42.9%).
However, a recent journal article in the Annals of Surgical Oncology stated that shave biopsies translate to a relatively small number of patients who have their T-stage increased (7.7%) or require a change in treatment recommendation (2.3%) after wide local excision. And so there was no significant difference in recurrence or survival rates between melanoma patients diagnosed with shave biopsy and other biopsy methods.
Ahmadi, O., Das, M., Hajarizadeh, B. et al. Impact of Shave Biopsy on Diagnosis and Management of Cutaneous Melanoma: A Systematic Review and Meta-Analysis. Ann Surg Oncol 28, 6168–6176 (2021)
TOTAL BODY PHOTOGRAPHY

Is there any benefit to performing skin photography or digital surveillance?
A recent article in the Australasian Journal of Dermatology compared the results of traditional melanoma surveillance, which involves regular full-skin examinations and immediate removal of suspicious lesions, to the results of two newer surveillance methods: total body photography (TBP) and sequential digital dermoscopy imaging (SDDI). They found that traditional surveillance resulted in a higher ratio of in situ to invasive melanomas (4.59:1) and a lower incidence of thick invasive melanomas (<1%) than TBP and SDDI. Delayed excision, which is inherent to photographic monitoring, carries at least some risk of melanoma progressing from a lower to a higher risk category.
This data raises the possibility that traditional skin examination and biopsy techniques (instead of photographic monitoring) may be safer and more effective.
Organ Transplants

Organ Transplantation
CHONDRODERMATITIS NODULARIS HELICIS

Chondrodermatitis Nodularis Helicis
In the Journal of Dermatologic Surgery, a novel treatment was proposed for Chondrodermatitis Nodularis Helicis (CDNH).
CDNH is a common chronic condition characterised by a painful nodule on the ear which may have accompanying crusting or ulceration.
CDNH is often difficult to treat or treatment only gives temporary benefit. Avoiding pressure is difficult to do when the lesion usually occurs on the favoured sleeping side. Surgical excision is often plagued by recurrence.
0.2 – 0.3 mL of Hyaluronic Acid (HA) was injected into the ear and found to provide significant relief from pain and clinical symptoms (including ulceration) in less than 1 – 2 weeks. Sometimes a second follow-up injection was required 2 weeks later if there was extrusion of HA material through a pre-existing ulcer.
No adverse events were noted other than the intentional visible bulging of the injected region. And these good results were achieved long term with one patient maintaining the benefit for 5 years!
INVERSE DERMOSCOPIC APPROACH

Inverse Dermoscopic Approach
In the Journal of the American Academy of Dermatology, a study showed significant increase in diagnosis of lentigo maligna (Hutchinson’s Melanotic Freckle) when traditional training for dermoscopic pattern analysis was compared with inverse approach training.
The dermoscopic features of actinic keratoses (sunspots), actinic lentigos or flat seborrhoeic keratoses (liver spots) are easy to identify. An inverse approach involves diagnosis by identifying the absence of these features.
Use of the inverse approach to dermoscopy outperformed traditional dermoscopic pattern analysis with diagnostic accuracy increasing by more than 60%!
